At one time, sawing off a gangrenous limb without anaesthetic was hailed as a medical breakthrough, mainly when the patient survived. Trepanning, too, was hailed as cutting-edge. That involved using a trephine to cut a hole in a patient's skull so the doctor could treat intracranial conditions. Trepanning is still practised today, but it first requires a series of diagnostic scans, and the cut-out part of the skull is replaced.
Until recently, patient care was less of a concern than triumphing over disease. That doesn't mean that saw-wielding surgeons of yore roamed the countryside, looking for people to cut. Plenty of people cared about patient comfort and well-being. We didn't have the technology or the means to ensure that care mattered as much as cure. Furthermore, collaborating with an insightful biology teacher can provide valuable context about the evolution of medical practices.
Today, we have vast stores of knowledge about drugs, chemicals and biological processes. They help inform doctors' choices of therapies and medical solutions for almost all our ills. We have fantastic, futuristic technologies to make science fiction a reality. But marrying technology to healthcare provokes:
- ethical debates about the future of Medicine
- an ongoing conversation about nutrition's role in health outcomes
- ideas of what personalized medicine should look like
- some of the past decade's most extraordinary medical breakthroughs
Currently, people at every level are chiming in about the threats and benefits artificial intelligence (AI) poses. Most project dystopic scenarios far into the future, but what about AI today? Let's examine how technology, in general, and specific AI applications can change healthcare concepts.
A biology tutor can use their expertise in medical breakthroughs to not only enrich students' understanding but also inspire them to learn outside of the classroom.

The Top Medical Breakthroughs of the Last Decade

Meet Alex Lewis. In November 2013, he went to bed early, feeling like he had a cold coming on. Instead, he had a bacterial infection that claimed all four limbs, his lips and his nose. As sepsis set in, his organs shut down, nearly costing him his life.
Alex's case is dramatic not just for his virulent infection but for technology's role in saving his life. In less than 24 hours, his legs had to be amputated as well as his left arm. Within days, his body, riddled with sepsis, started shutting down. His doctors put him in a medically-induced coma.
Had Alex contracted this infection a decade earlier, his prognosis would have been less encouraging. Even if he had survived the onslaught, living as a disfigured quadruple amputee would have been challenging. But advances in robotics and bionics mean that Alex has restored limb functionality. As the technology improves, upgrades to his prosthetics will allow him an even greater quality of life.
Former cyclist Gert-Jan Oksam knows how it feels to regain mobility and functionality. He lost the use of his legs a dozen years ago, but now, thanks to a dual brain and spinal implant, he can walk again. Three years ago, the first brain implants restored vision to blind people, but restoring mobility was more challenging. This complex procedure was only possible after the past decade's medical breakthroughs.
The Ethical Debate Over Gene Editing
In 1953, James Watson and Francis Crick discovered the DNA helix. Thirty years later, scientists found that Huntington's disease has a genetic origin. Seven years later, science discovered cancer susceptibility reflected in the human genome.
Perhaps, until Huntington's and cancer gene discoveries, people thought how and why they got sick was random chance. Discovering that humans are susceptible to certain diseases because of their genetic makeup was a giant leap forward. It suggested that a thorough understanding of the human genome could eradicate the disease. Thus, in 1990, the Human Genome Project began.
Historians, philosophers and lawmakers were quick to slam on the brakes. Nearly a century before, the eugenics movement came into vogue. This movement was meant to ensure a population of genetically superior humans. The idea was fraught with racist and classist overtones.
Time, technology and tolerance saved the day. In 1959, the genetic cause of Down's Syndrome was discovered. No one believed it wise to change that chromosome. Over time, specific instances of gene editing gained approval, but a recent event has brought that debate back to the foreground.
How Sound Nutrition Can Help Prevent Disease

If our genes make us more likely to get sick, what we put in our bodies must play a part, too. For decades, the medical community has recommended what we should eat and drink. But people keep getting sicker and fatter.
There must be a disconnect between what we're told to eat and what is healthy. For instance, eating grains has long been standard dietary advice, but nobody has said which grains. And how they should be processed to keep them nutritious. And everyone is on about calories; how many you take in and how many you burn up.
Calorie advice is exceptionally misleading. Not all calories are the same; some are empty, and some take longer to burn off. Individual bodies respond differently to different types of calories, too. Focusing on caloric intake often means overlooking nutrition.
Dietary fat is essential to maintaining your physical and mental health. But fat has long been demonised, too, with the 'eat fat, get fat' tagline attached to every fat discussion. The opposite is true; new studies show that eating more fat can help you slim down. Furthermore, diets rich in healthy fats return lower cancer rates, including prostate, breast and colon cancers.
Fat studies offer even more good news: dietary fats also help stave off a range of mental conditions. High-fat diets show a decreased cognitive decline, memory loss due to ageing and even depression. Considering that developed societies have been on a 50-year fat-free, calorie-counting binge, all of this is good news.
It's also intriguing. Heart disease, Type II diabetes, and obesity numbers have steadily ticked up over that time. So too, has the number of people with mental health issues and depression. And since the 1990s, cancer rates have increased—specifically breast and colon cancers and kidney, liver and pancreas cancers.
Research proves the link between nutrition and disease, but the picture is incomplete. Our environment plays a role in shaping our health, too. Pollution, toxins and how physically active we are all depend on where and how we live. So does our genetic profile.
Like every other aspect of our health, taking a one-size-fits-all approach to individual nutritional needs doesn't work. You should discover what nutrition your body needs to prevent disease and protect your mental health. Our companion article gives you tips to find that out.
Personalized Medicine: The Healthcare of the Future
'One size fits all' medicine compels the most aggressive treatments. But patients come in all shapes, sizes and genetic profiles. Many don't fare well under aggressive treatment. And sometimes, the disease recurs.

Medical personnel have long been frustrated at the hit-and-miss nature of their work. Surgery, chemo and radiation therapy may send cancer into remission, but why does it return? Nobody here blames the nurses or physicians. But maybe it's time to start treating the patient instead of the disease.
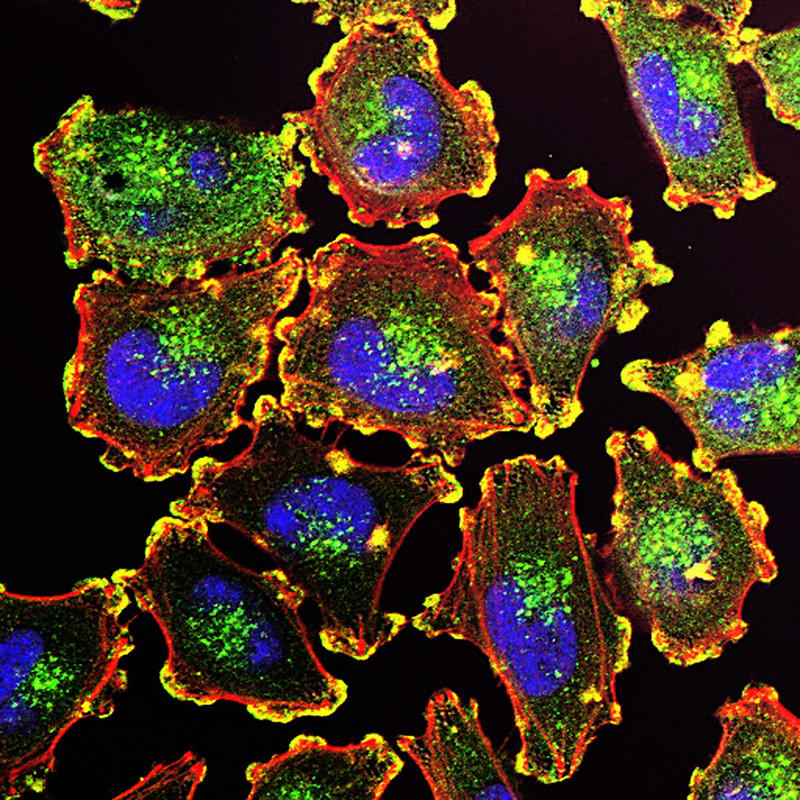
That's the philosophy driving the move towards personalized medicine. This AI-assisted initiative considers the patient before looking at what ails them. Personalized medicine looks at individual genetic profiles to help decide a treatment plan. It also looks at other factors, such as their diet and environment, to determine which therapy might be the most effective.
Going through the advancements in medicine under the guidance of a biology tutor will help you connect theoretical knowledge with practical applications, illustrating how these breakthroughs can revolutionise patient care.
Let's say a patient presents with high blood pressure, high blood glucose levels and high triglycerides. They're also obese - 'apple shaped', meaning they have a large abdomen. Typically, a doctor would prescribe a medicine for each condition and advise the patient to lose weight. There likely won't be a referral to a nutritionist or dietician.
Metabolic syndrome, the condition those symptoms describe, is a lifestyle disease. However, some metabolic disorders are genetic. So prescribing various medications without first considering genetic or environmental conditions is ineffective.
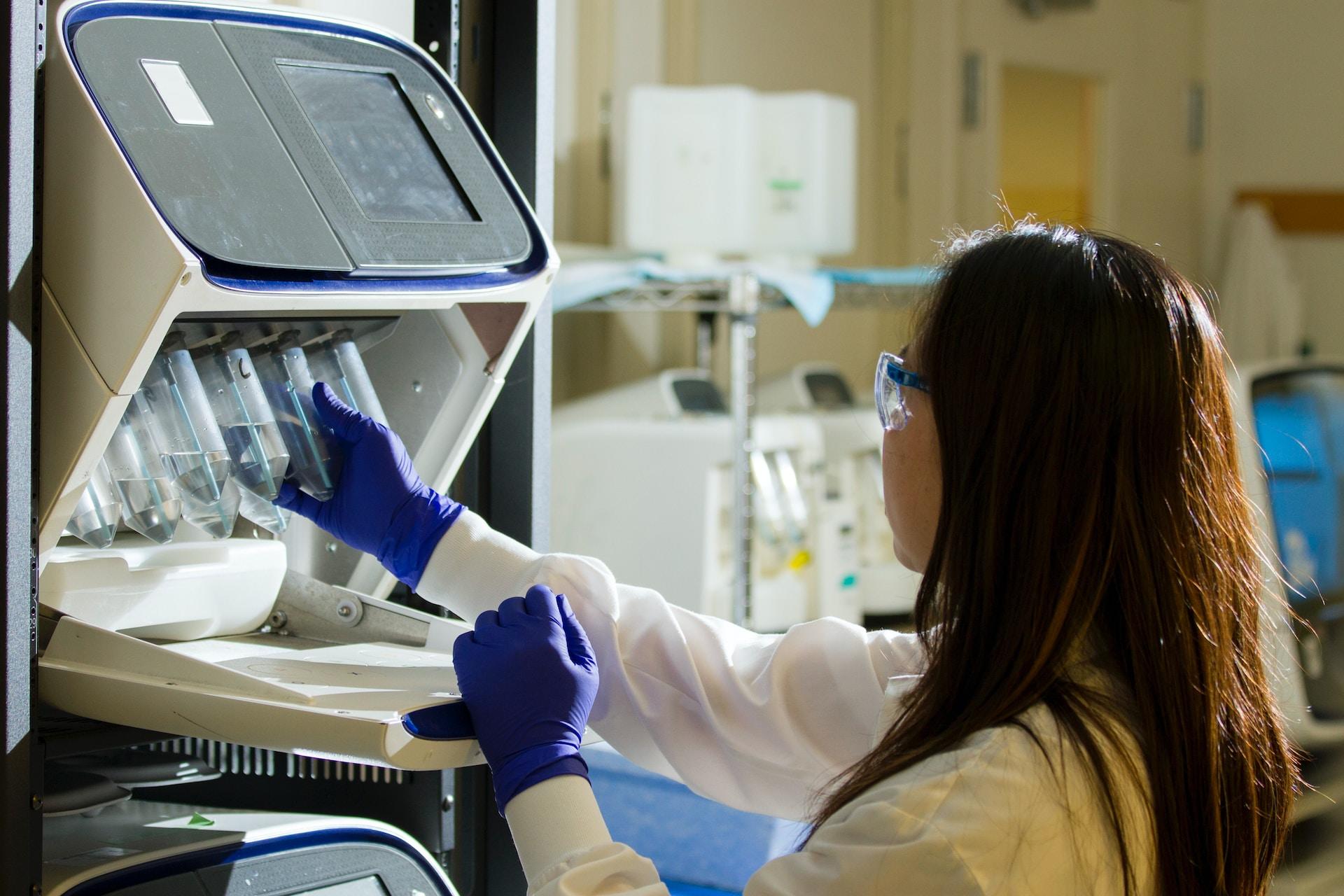
Technology-assisted diagnosis considers the patient first and treatment options second. Knowing the patient's genetic profile means AI may rule out all metabolic conditions. The patient might already use a wearable device that reports their calorie intake and activity levels. With that information, AI could quickly conclude that lifestyle choices cause this quartet of symptoms.
Doctors are constantly harried to treat more patients, cure more diseases, do more research and publish more papers. They work long hours, trying to get it all done. Physicians often only have a few minutes with each patient before scuttling off to the next examination room. Imagine how much more productive those few minutes would be if the doctor had AI assistance.
But personalized healthcare doesn't make only doctors' work more accessible. It lets you take control of your healthcare, too. Wearables are one such instance; you can track your markers to fine-tune your health regimen. Plugging that data into your doctor's AI-driven platform gives you a 'patient first' diagnostic and treatment system.
Summarise with AI: